Building an enterprise-level AI module for travel insurance claims is complex. Claims processing requires handling diverse data formats, interpreting detailed information, and applying judgment beyond simple automation.
When developing Lea’s AI claims module, we faced challenges like outdated legacy systems, inconsistent data formats, and evolving fraud tactics. These hurdles demanded not only technical skill but also adaptability and problem-solving.
In this article series, we’ll share the in-depth journey of building Lea’s AI eligibility assessment module: the challenges, key insights, and technical solutions we applied to create an enterprise-ready system for travel insurance claims processing.
Challenge : Error Handling and Dynamic Risk Assessment
Key Learnings:
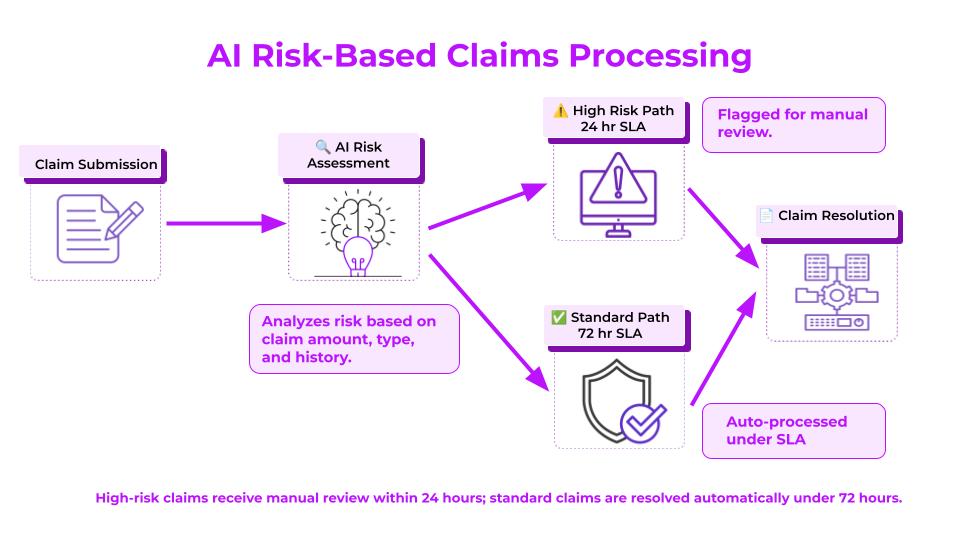
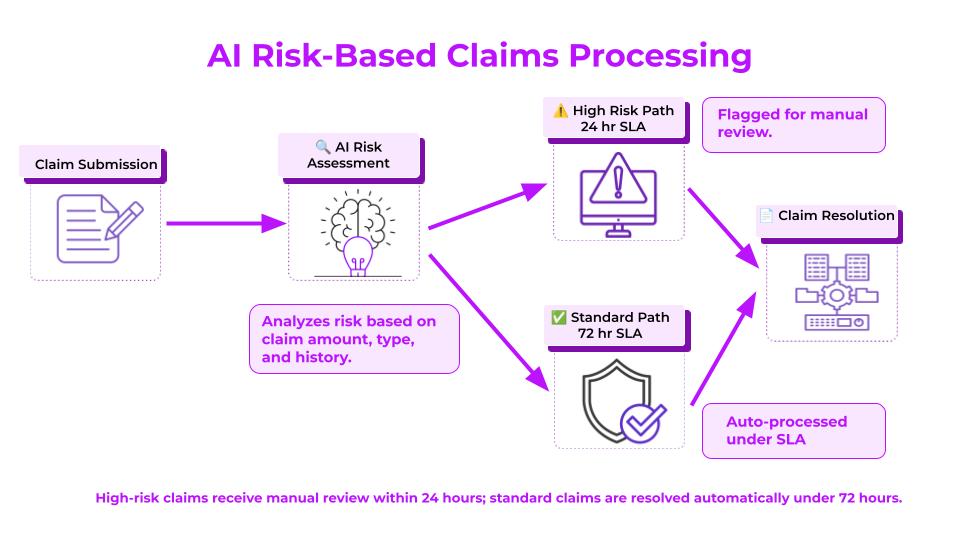
- Dynamic Risk Assessment for Efficient Claims Processing: Real-time risk assessment evaluates each claim’s risk level, flagging high-risk cases for immediate review to allocate resources efficiently and reduce processing delays.
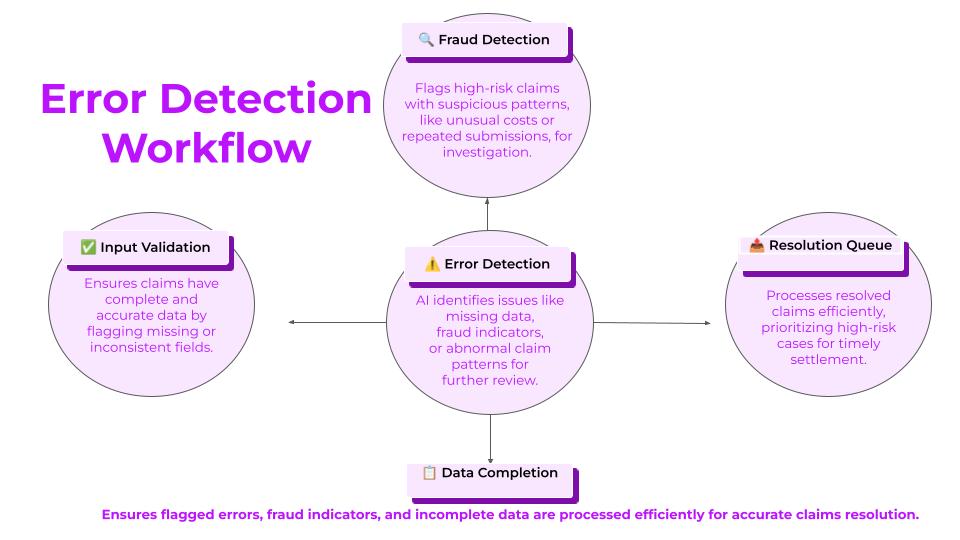
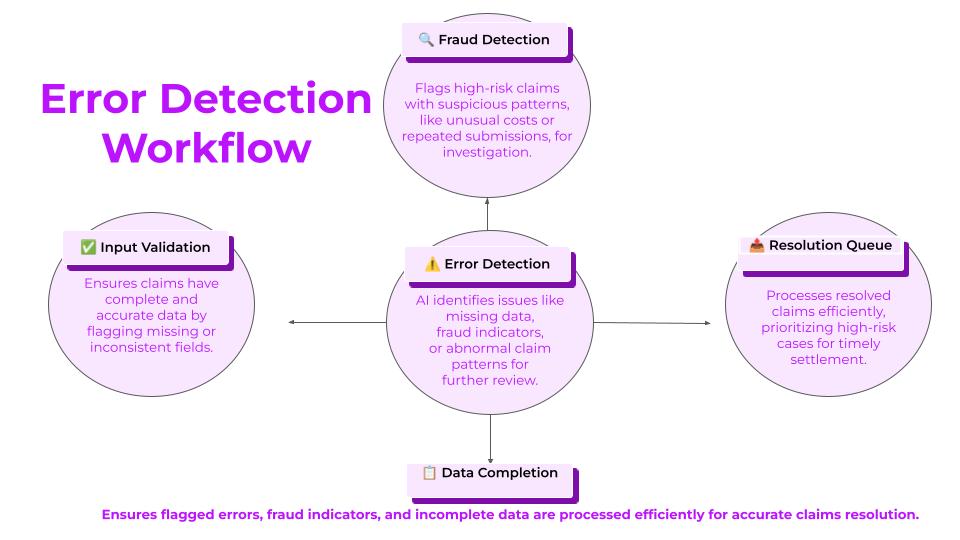
- Proactive Error Handling for Greater Accuracy: With categorized alerts, layered workflows, and real-time notifications, the system detects and manages errors promptly, ensuring claims with missing data or fraud indicators are handled with targeted attention.
- Operational Continuity with Redundant Processing Paths: Fallback processing and human-in-the-loop feedback mechanisms maintain claims processing during high demand, ensuring data accuracy, AI improvement, and uninterrupted service.
In travel insurance, claims processing requires managing diverse data and dynamically allocating resources. This system provides AI-driven risk assessment, operational continuity, and error handling, optimizing processing for high-risk or complex claims with minimal delays.
Real-Time Risk Assessment and Dynamic Escalation Protocols
Our claims module assesses risk using attribute-based analysis (e.g., claim amount, treatment type, location, claimant history) to identify high-risk claims and route them accordingly. This approach ensures high-risk cases receive detailed review and that processing remains efficient.
- Automated High-Risk Routing: Claims that exceed specific thresholds—such as those with high claim amounts or involving non-standard treatments—are automatically flagged for human review. For instance, a high-cost medical claim from a remote location might be flagged due to regional cost variations, ensuring alignment with policy standards and regional expectations.
- Layered Workflow Paths for Targeted Review: Decision-tree logic classifies and routes claims based on specific error types:
- Fraud Indicators: Claims with suspicious patterns, such as a medical bill that deviates significantly from local treatment costs, are routed to the fraud analysis team.
- Incomplete Data: Claims missing essential information (e.g., an unspecified “incident_location”) are directed to data verification to gather necessary details.
- Each error type is assigned a unique handling protocol, directing claims to appropriate experts without unnecessary steps and minimizing processing delays.
Escalation Protocols for Efficient Resource Allocation
Our escalation protocols use risk-based and time-based criteria to prioritize claims effectively.
- Risk-Based Escalation: Claims surpassing defined risk levels (e.g., “risk_score” above 90) are escalated to senior assessors, ensuring critical cases receive timely attention and maintaining processing integrity.
- Time-Based Escalation: Claims unresolved within set time limits (e.g., “time_in_queue” > 24 hours) are flagged for immediate action to prevent workflow backlogs.
Real-Time Alerts and Categorized Error Notifications
Prompt notifications are essential for managing errors efficiently. The system classifies and prioritizes alerts by type, offering clear visibility into flagged issues.
- Instant Notifications: Real-time alerts provide key metadata for flagged claims, such as “alert_type” (e.g., High Risk) and “priority_level” (e.g., Critical), enabling immediate responses for urgent cases.
- Example: A critical notification might be triggered for a high-cost emergency evacuation claim due to a medical emergency on a remote island, prompting rapid response from the claims team.
- Error Type Categorization: Alerts are grouped by categories, such as potential fraud, missing data, or excessive claim value. For instance, a claim lacking the “incident location” due to rushed submission from a traveler would be categorized as “missing data” and directed to verification, allowing the team to address high-priority cases quickly and refine model parameters based on recurring patterns.
Human-in-the-Loop (HITL) Interactive Review Dashboard
To refine AI-driven claims processing with human expertise, the HITL dashboard centralizes flagged claims for detailed review. The dashboard displays AI’s flagging rationale, risk indicators, and required actions, supporting informed decisions by experts.
- Feedback Loop for Continuous Improvement: Reviewers label incorrect flags as “false positives” directly in the dashboard, feeding this feedback into the AI model to improve accuracy. For instance, repeated feedback on common medical procedure claims abroad helps refine fraud detection parameters, reducing false positives and improving claim processing efficiency.
Data Consistency and Error Logging for Root Cause Analysis
To maintain data reliability, each flagged claim is logged in a centralized error database, tracking flagging reasons and identifying recurring patterns. This log supports root cause analysis for better AI accuracy and error handling.
- Root Cause Analysis for AI Model Tuning: Analysts review error logs to refine model parameters and reduce similar issues in future claims. For example, error logging revealed that certain high-cost overseas medical claims frequently triggered fraud alerts. Further investigation showed that these claims were legitimate, resulting from specialized services in specific regions. Adjustments were made to account for these variations, reducing unnecessary escalations and improving fraud detection accuracy.
Operational Continuity with Redundant Processing Paths
Ensuring uninterrupted service for high-priority claims is essential. The system’s redundancy setup provides fallback processing paths during AI downtime.
- Backup Routing for Claims Processing: In case of AI downtime, high-priority claims are rerouted to human reviewers to ensure continuous processing.
- Automated Reprocessing of Human-Reviewed Claims: After human review, claims re-enter the AI pipeline to capture manual adjustments, preventing similar issues from recurring.
Edge Cases in AI-Driven Claims Processing
Our system’s error-handling and continuity framework addresses various complex cases often encountered in travel insurance:
- High-Value Claims: Large emergency treatment claims abroad, such as those over $20,000, are escalated immediately for validation due to higher risk.
- Incomplete Data: Claims missing essential fields, like “incident_location,” are flagged for verification.
- Non-Standard Treatments: Claims involving alternative treatments, like “acupuncture,” are flagged for additional review due to varying coverage terms.
- Rare Events: Claims related to uncommon events, such as volcanic eruptions, are flagged for specific policy exclusion reviews.
- Policy Upgrades Mid-Trip: For claims tied to mid-trip policy changes, the system checks “policy_change_date” against “incident_date” to verify eligibility.
- Multi-Destination Itineraries: Trips covering multiple destinations are segmented to verify coverage for each location, ensuring thorough claims processing.
Benefits of Our Comprehensive Claims Management System
- Seamless Continuity and Error Management: Fallback workflows, escalation protocols, and categorized alerts help maintain efficient claims processing, even during high demand.
- Enhanced AI Accuracy through Continuous Feedback: The HITL feedback mechanism allows for ongoing model adjustments, reducing false positives and improving decision accuracy.
- Reduced Backlogs with Dynamic Task Management: Real-time escalations and task routing streamline complex claims, reducing bottlenecks and enabling faster resolution.
Ancileo’s system provides an approach to AI-driven claims processing, integrating real-time risk assessment with proactive error handling. This scalable design supports travel insurers in managing complex, high-stakes claims accurately and efficiently, tailored to the needs of the travel insurance industry.